BCMA IV-Medication Administration: A Safety and Efficiency Review
Lisa Gangol. RN, BSN. Beckton Dickinson. Senior Clinical Resource Consultant. Medication Management Solutions. Middle East, North Africa and Turkey. Lisa.Gangol@bd.com
Larry Neal. Regional Marketing Manager, Medication Management Solutions. Becton Dickinson. Europe, Middle East and Africa. Larry.Neal@bd.com.
James Waterson. RN, M.Med.Ed. MHEc. Becton Dickinson. Medical Affairs Manager, Middle East & Africa. James.Waterson@bd.com
The Issue is Serious
Medication errors occur at all stages of the medication management process, but approximately 34% of preventable medication errors occur during administration and most errors that occur during administration are not intercepted.1 The World Health Organization (WHO) has identified that a leading cause of preventable harm in healthcare systems is linked to unsafe medication practices and medication errors. The costs associated with medication errors have been estimated at approximately $42 billion annually, excluding lost wages, lost productivity, and indirect healthcare costs. The WHO identified that medication errors occur when prescribing, transcribing, dispensing, administration and monitoring practices are undertaken in weak medication systems and when human factors such as fatigue, poor working conditions, workflow interruptions are present.2
‘The Big Three’
The position of the American Society of Hospital Pharmacists, the European Association of Hospital Pharmacists, and the Institute of Safe Medication Practices is very clear. Adoption of Barcode Medication Administration (BCMA) in all areas of health systems in which medications are used is recommended, particularly in areas with a likelihood of limited patient stay, such as the Emergency Department, perioperative areas, infusion and dialysis centers, and outpatient areas.3,4,5
A further recommendation is that compliance and metric data is routinely collected to evaluate the utilization and effectiveness of BCMA, such as scanning compliance rates, and alert overrides.
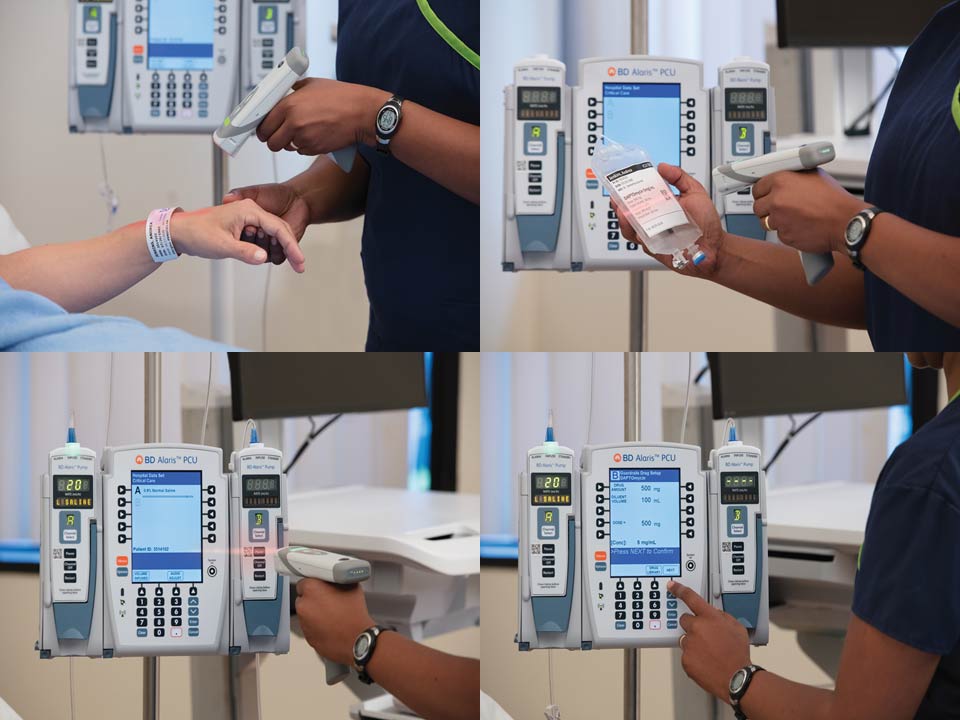
A System Defence: Zoom-In on IV-Medication Error Prevention
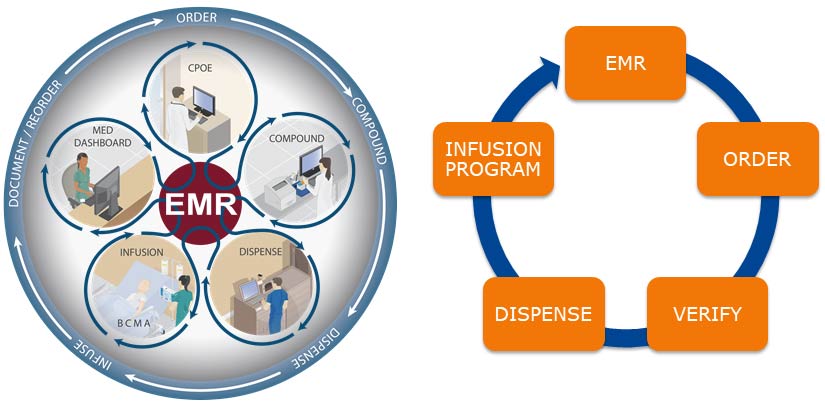
Closed-loop IV-medication management systems have been identified as a vital component of systematic defenses to prevent intravenous IV-medication errors.6
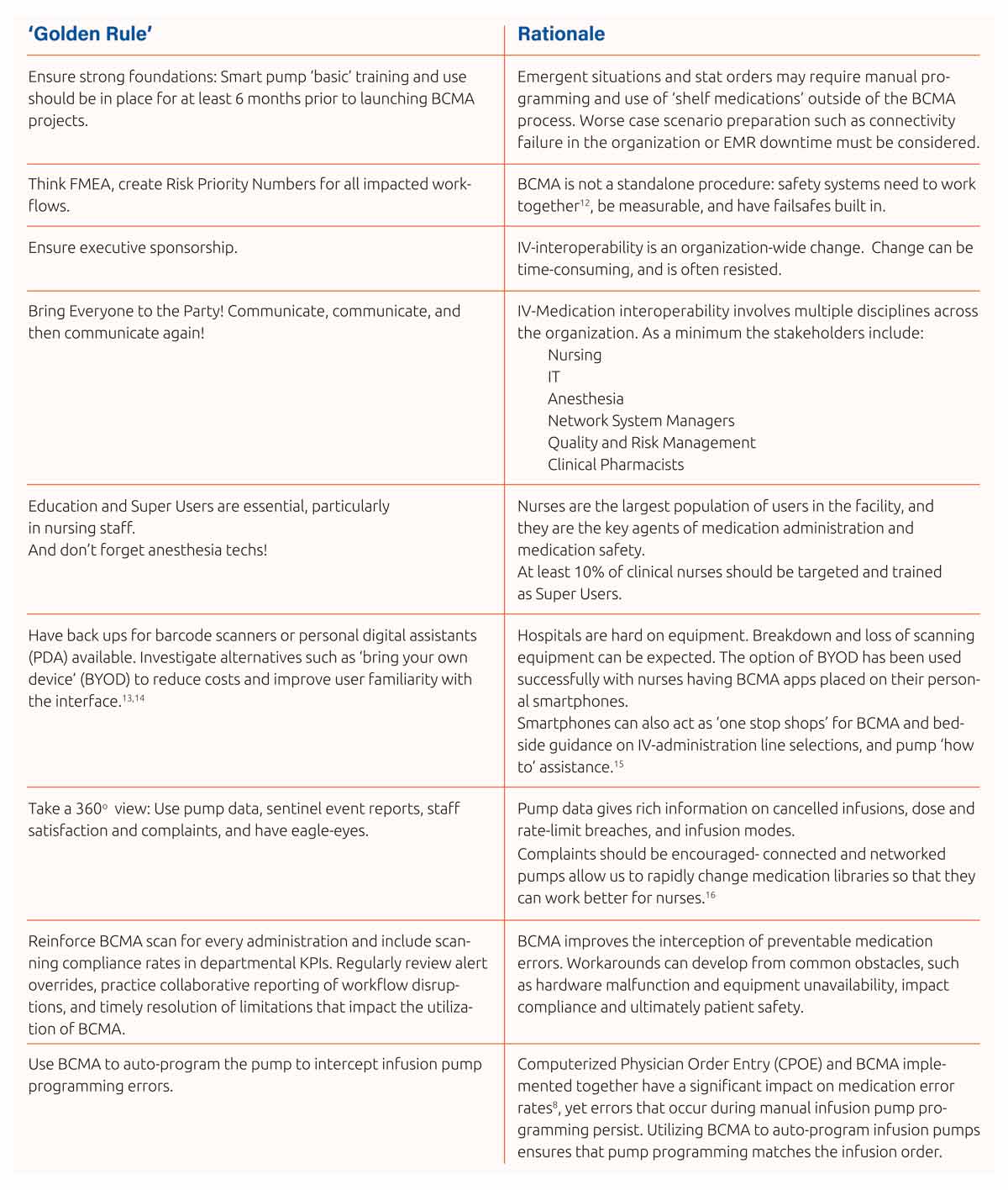
Nurses are the primary users of BCMA and nursing involvement, along with nursing executive sponsorship of any new BCMA project across an organization is essential for successful implementation.3 IV-pump manufacturers should offer a clinical appraisal or ‘walkthrough’ service, where medication workflows are examined, and planning to prevent potential unwanted workarounds or likely deviations from correct procedures can be made. Workarounds, overrides, and ‘clinical variation’ are consistently noted in the literature as major causes of medication error even in advanced systems with multiple safeguards.7,8
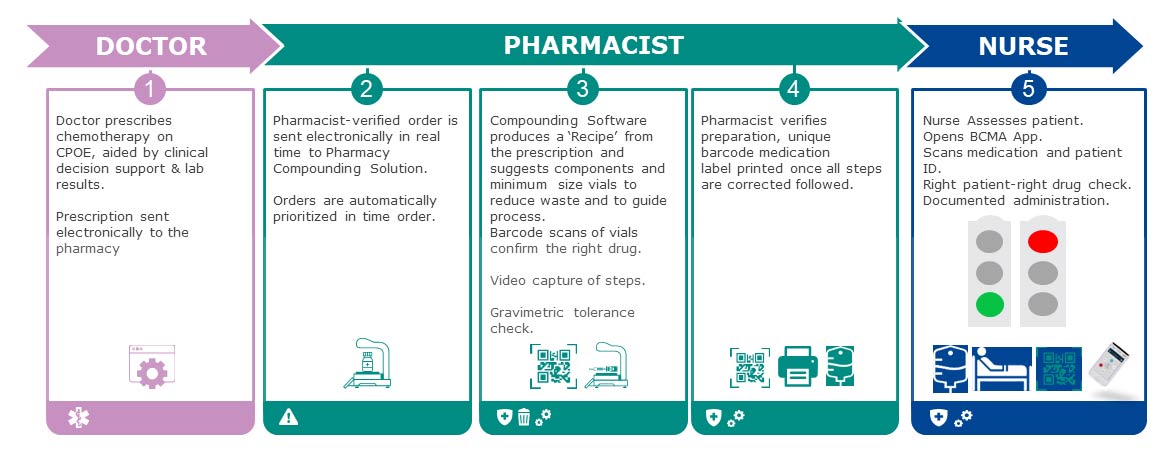
Typical workarounds include affixing patient identification bands away from the patient and carrying pre-scanned medications on charts.8 Ensuring consistent patient-specific IV-medication availability from the compounding room to avoid the use of non-coded ‘shelf medications’, and ensuring that the medication carries the key information required for BCMA in the barcode is vital if workarounds are to be reduced:
Key Information for BCMA Medication labels and to be transmitted to the IV-closed loop safety checks via the barcode
- Patient ID
- Medication ID
- Order String Identifier
- Total Dose
- Total Volume
- Dose Units
A fully integrated prescription-compounding and administration system has been shown to substantially improve IV-medication safety and to reduce administration time.9 It has also been suggested that ‘guidance’ is not enough and forcing functions such as hard-stops have far more value in supporting safe medication prescription, preparation and administration.9
The Learning Curve: Human-BCMA System Interaction
Understanding why BCMA is of such value in IV-medication safety is made easier once we look at the types of cognitive failures that most commonly lead to error:
Cognitive Failure:10
- Lapses and slips, routine activities are accomplished quickly with minimal attention requirements.
- Performance based errors: alternative focus, interruptions, and lapses which contribute to errors of omission due to ‘reduced intentionality’.
- Rule-based mistakes: an inadvisable rule is applied, developed from misunderstanding of a problem and the conditions that govern it.
There is always a ‘lag’ in obtaining the full benefit of medical technology after introduction to a facility,11 but this can be shortened for Electronic Medical Record based IV-medication interoperability projects by adherence to some fundamental rules which as BD clinicians we have observed during IV-medication interoperability installations in our region and in the United States:
Error Reduction and BCMA Utilization
IV-Medication error is a complex phenomenon and IV-medication BCMA interoperability impacts the medication chain at multiple points as it closes the loop and links administration more directly to the prescription than any other current system.
Due to this complexity ‘simple numbers’ such as a 43.5%17 reduction in reported medication administration errors overall after the implementation of BCMA and need to be scrutinized carefully (though this is encouraging as well as the lack of patient harm events attributed to medication administration error following BCMA implementation17).
Studies that take a longer and more complex look at the medication safety landscape within an organization are of real value in ascertaining the real gains made.18 Using an interrupted time series analysis (ITSA) model Thompson et al. estimated that there were 30% fewer events post-BCMA introduction than there would have been without the intervention.17
In an Emergency Department study a 10.8% reduction in medication error rates and 21% reduction in the average number of medications given in error per chart was observed.19 As noted in the introduction, BCMA may have added value in high-turnover care areas.3,4,5
Impact of BCMA on Direct Patient Care
One time-motion study looked at the effect of BCMA on nursing activities in critical care. Time spent on direct patient care activities increased with the use of BCMA technology, while time spent on administration activities decreased. Nurses were able to complete administration activities faster during the BCMA phase, which was attributed to ease of access to patient information and medication resources.20
In one study of a well-functioning medication chain the average time required to administer IV-oncology medications dropped from over 6 minutes to 41 seconds.9
Optimizing the System
Medication error reports giving an overview of events and displayed warnings and overrides derived from the BCMA system have been used to optimize multiple stages of the medication management process: revision of standard administration times, improved storage strategies for medications in nursing-unit cabinets, separation of look-alike-sound-alike medications, and resolution of formulation discrepancies in the IV-clean room. 21
Drilling down into this data allows for targeting of education for nursing units not utilizing BCMA properly, identification of order-entry discrepancies and bar code-label quality concerns.21
In Conclusion
BCMA sits within a complex interaction of systems, humans, skills, and procedures. The standardization of workflows and reduction of clinical variability across all stages of medication management that it drives is recommended by the ‘Big Three’3,4,5. When coupled with optimal utilization, barcode medication administration has demonstrated successful reduction of preventable medication administration errors for hospitalized patients. 22
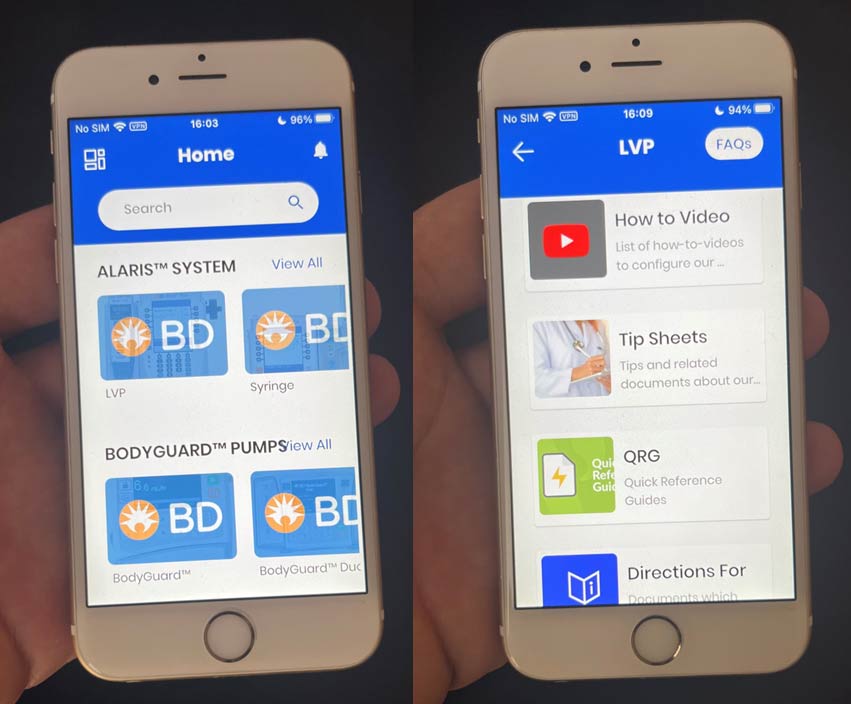
The BD Clinical App is available for iOS and Android devices.


References:
1. Bates, D.W., Cullen, D.J., Laird, N., Petersen, L.A., Small, S.D., Servi, D., Laffel, G., Sweitzer, B.J., Shea, B.F., Hallisey, R., Vilet, M.V., Nemeskal, R., Leape, L.L., Bates, D., Hojnowski-Diaz, P., Perycki, S., Cotugno, M., Patterson, H., Hickey, M. Edmondon, A. Incidence of Adverse Drug Events and Potential Adverse Drug Events: Implications for Prevention. Journal of the American Medical Association, 1995, 274(1), 29-34. DOI: 10.1001/jama.1995.03530010043033
2. World Health Organization (WHO). 10 Facts about Patient Safety. World Health Organization. (9 March 2019). https://www.who.int/news-room/facts-in-pictures/detail/patient-safety
3. Dabestani, A.T. & Perry, A.B. ASHP Statement on Bar-Code-Enabled Medication Administration Technology. American Journal of Health-System Pharmacists, 2009, 66, 588-590. DOI: 10.2146/ajhp080414
4. Batista, A., Polidori, P., & Kohl, S. Position paper on patient safety. European Journal of Hospital Pharmacists, 2021, 28, 129-132. DOI: 10.1136/ejhpharm-2019-001924
5. Institute of Safe Medication Practices (ISMP). (2022). ISMP Targeted Medication Safety Best Practices for Hospitals. ISMP. https://www.ismp.org/guidelines/best-practices-hospitals
6. Kuitunen, S.K., Niittynen, I., Airaksinen, M., & Holmstrom, A. Systemic Defenses to Prevent Intravenous Medication Errors in Hospitals: A Systematic Review. Journal of Patient Safety, 2021, 17(8), e1669-e1680. www.journalpatientsafety.com
7. Gann, M. How informatics nurses use bar code technology to reduce medication errors. Nursing 2015, 60-66. DOI: 10.1097/01.NURSE.0000458923.18468.37
8. Stolic, S., Ng, L., & Sheridan, G. Electronic medication administration records and nursing administration of medications: An integrative review. 2022. Collegian, 1-27.
9. Meren ÜH, Waterson J. Evaluating An Automated Compounding Workflow Software for Safety and Efficiency: Implementation Study. JMIR Hum Factors. 2021 Nov 2;8(4):e29180.
10. Mattox, E.A. Strategies for Improving Patient Safety: Linking Task Type to Error Type. Critical Care Nurse, 2012. 32(1), 52-60. DOI: 10.4037/ccn2012303
11. Tarricone R, Callea G, Ogorevc M, Prevolnik Rupel V. Improving the Methods for the Economic Evaluation of Medical Devices. Health Econ. 2017 Feb;26 Suppl 1:70-92.
12. Wiegmann DA, Wood LJ, Cohen TN, Shappell SA. Understanding the “Swiss Cheese Model” and Its Application to Patient Safety. J Patient Saf. 2022 Mar 1;18(2):119-123.
13. Darawad, M.W., Othman, E.H., & Alosta, M.R. Nurses’ satisfaction with barcode medication-administration technology: Results of a cross-sectional study. Nursing & Health Sciences, 2019, 21, 461-469. DOI: 10.1111/nhs.12620
14. Al-Jaber R, Samuda N, Chaker A, Waterson J. Critical Care Nurses’ Knowledge of Correct Line Types for Administration of Common Intravenous Medications: Assessment and Intervention Study. JMIR Form Res. 2022 Apr 26;6(4):e36710.
15. Foo, G.T., Tan, C.H., Hing, W.C., & Wu, T.S. Identifying and quantifying weaknesses in the Closed Loop Medication Management System in reducing medication errors using a direct observational approach at an academic medical centre. Journal of Pharmacy Practice and Research, 2017, 47, 212-220.
16. Waterson J, Al-Jaber R, Kassab T, Al-Jazairi AS. Twelve-Month Review of Infusion Pump Near-Miss Medication and Dose Selection Errors and User-Initiated “Good Save” Corrections: Retrospective Study. JMIR Hum Factors. 2020 Aug 11;7(3):e20364.
17. Thompson, K.M., Swanson, K.M., Cox, D.L., Krichner, R.B., Russell, J.J., Wermers, R.A., Storlie, C.B., Johnson, M.G., & Naessesn, J.M. Implementation of Bar-Code Medication Administration to Reduce Patient Harm. Mayo Clinic Proceedings: Innovations, Quality, & Outcomes, 2018, 2(4), 342-351.
18. Schaffer AL, Dobbins TA, Pearson SA. Interrupted time series analysis using autoregressive integrated moving average (ARIMA) models: a guide for evaluating large-scale health interventions. BMC Med Res Methodol. 2021 Mar 22;21(1):58.
19. Gauthier-Wetzel, H.E. Barcode Medication Administration Software Technology Use in the Emergency Department and Medication Error Rates. CIN: Computers, Informatics, Nursing, 2022, 40(6), 382-388.
20. Dwibedi, N., Sansgiry, S.S., Frost, C.P., Dasgupta, A., Jacob, S.M. Tipton, J.A. & Shippy, A.A. Effect of bar-code-assisted medication administration on nurses’ activities in an intensive care unit: A time-motion study. American Journal of Health-System Pharmacists, 2011, 68, 1026-1031. DOI: 10.2146/ajhp100382
21. Paoletti, R.D., Suess, T.M., Lesko, M.G., Feroli, A.A., Kennel, J.A., Mahler, J.M., & Sauders, T. Using bar-code technology and medication observation methodology for safer medication administration. American Journal of Health System Pharmacists. 2007, 64, 536-543.
22. Skog J, Rafie S, Schnock KO, Yoon C, Lipsitz S, Lew P. The Impact of Smart Pump Interoperability on Errors in Intravenous Infusion Administrations: A Multihospital Before and After Study. J Patient Saf. 2022 Apr 1;18(3):e666-e671.














