Automation in Outpatient Medication Dispensing: Regional Experiences and Potential
James Waterson. RN, M.Med.Ed. MHEc. Medical Affairs Manager. Becton Dickinson, Medication Management Solutions. Middle East and Africa.
Maged Farrag BSc, ACIM. Business Development Manager. Medication Management Solutions. Becton Dickinson. Kingdom of Saudi Arabia.

An article submitted to the American journal of hospital pharmacy long ago in 1967 identified how ‘outpatient visits are increasing at a rapid rate and administrative adjustments will be needed to handle larger outpatient prescription volumes.’ The author laid out how, ‘new methods and procedures must be developed to reduce patient waiting time, provide the physician and the pharmacist with information pertinent to drug therapy and increase productivity through the elimination of administrative detail which can be handled better through automation’.1
The situation remains not dissimilar in 2022, some fifty-five years later. Outpatient visits continue to rise year-on-year, with increasingly complex patients being handled by these departments. Globally, there has been a drive towards automation in healthcare to help handle the constantly increasing workload, and to allow for the redeployment of our limited numbers of highly qualified staff away from routine tasks and towards more constructive engagement with patients.
There is also considerable political and financial pressure on healthcare decision-makers to optimize the utilization of resources and to improve services for patients, whilst ensuring that any automation and technology that is deployed definitively adds quantifiable health-economic value. The size of any initial investment in health technology and automation is inevitably significant and requires substantial decisions to be taken about funding, the need for change, and required re-engineering of a facility’s infrastructure and established hospital and department procedures, policies, and workflows.
Generally speaking, the areas in which automation may make a difference can be assessed through direct metrics such as average time from prescription order to dispensing, completeness of medications dispensed versus prescriptions, expired inventory, average inventory stock levels, turnaround of unused or uncollected medications into circulation, number of mislabelling or prescription discrepancy events caught, time taken in completing regular inventory, and the percentage of missing medications identified.

More intangible metrics such as the impact of automation on freeing pharmacists from non-valued added tasks, which might allow for ‘ringfencing’ of pharmacist time for patient counselling and education, which may assist in improved patient medication adherence and a reduction in medication error at home related readmissions2 are more difficult to apply, but patient satisfaction studies with the quality of pharmacy services can help triangulate this and specialist questionnaires related to the likelihood of a patient complying with medication regimens such as the Morisky-Green-Levine Medication Adherence Scale can be used.
Studies and meta-analyses related to automation processes for inpatient environments have been conducted; some of these can be extrapolated to the outpatient department but only with the caveat that while the two settings share some elements, there are also distinct differences in workflow challenges, safety concerns, service elements, and staffing.

A relatively recent systematic literature review of automated and semiautomated drug distribution systems in acute care hospitals evaluated effectiveness in terms of medication safety, time, and costs of medication management3. A general conclusion was that patient safety improved with automation, and that highly centralized systems for dispensing saved more time than decentralized arrangements.
In terms of medication picking, a key aspect of robotic pharmacy systems, a recent UK study conducted in the last quarter of 2019 showed that lookalike-soundalike (LASA) errors represented 25.9% of the total of all human dispensing errors 4. LASA medications is an area where barcode reading by machine would be expected to be potentially error-free.
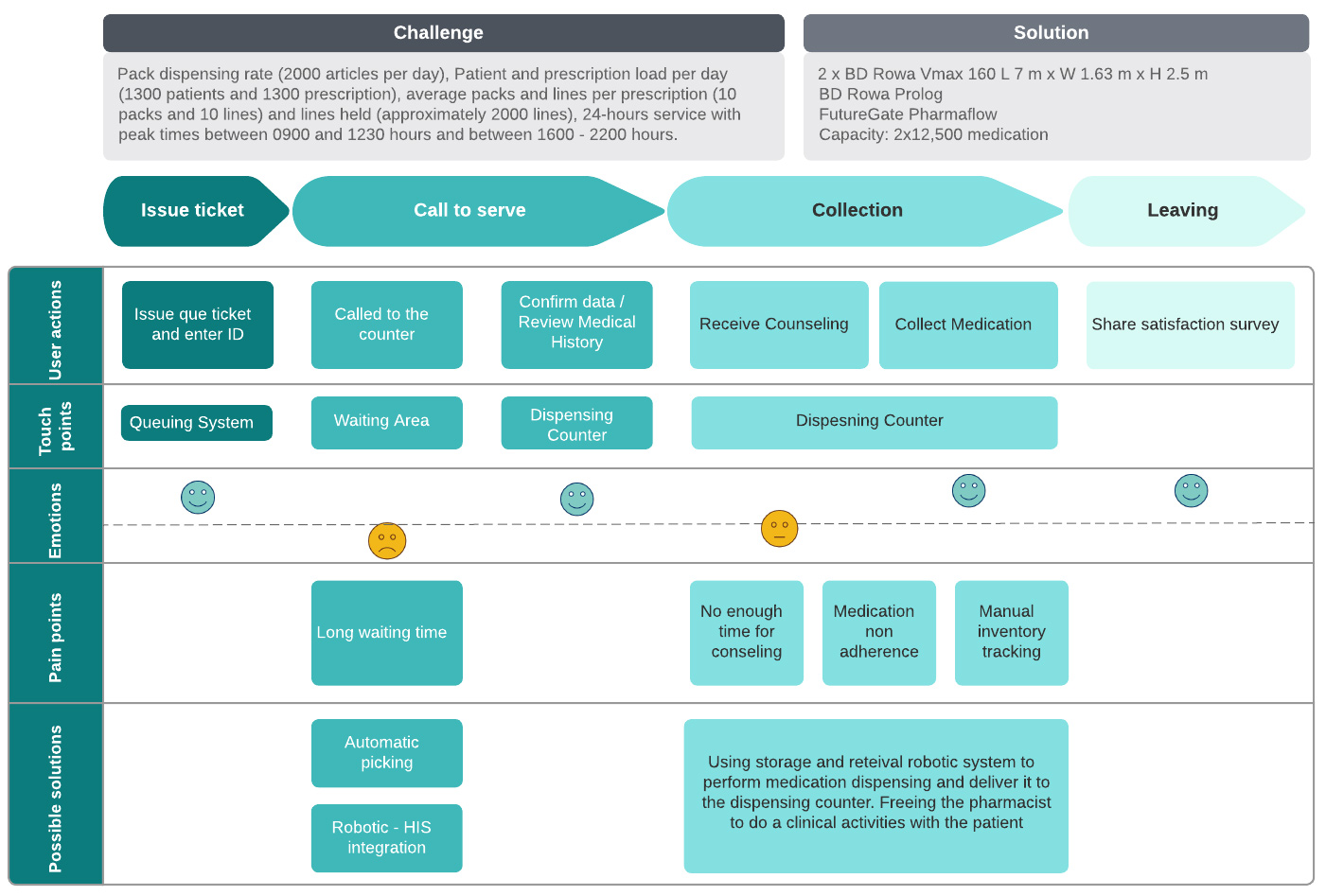
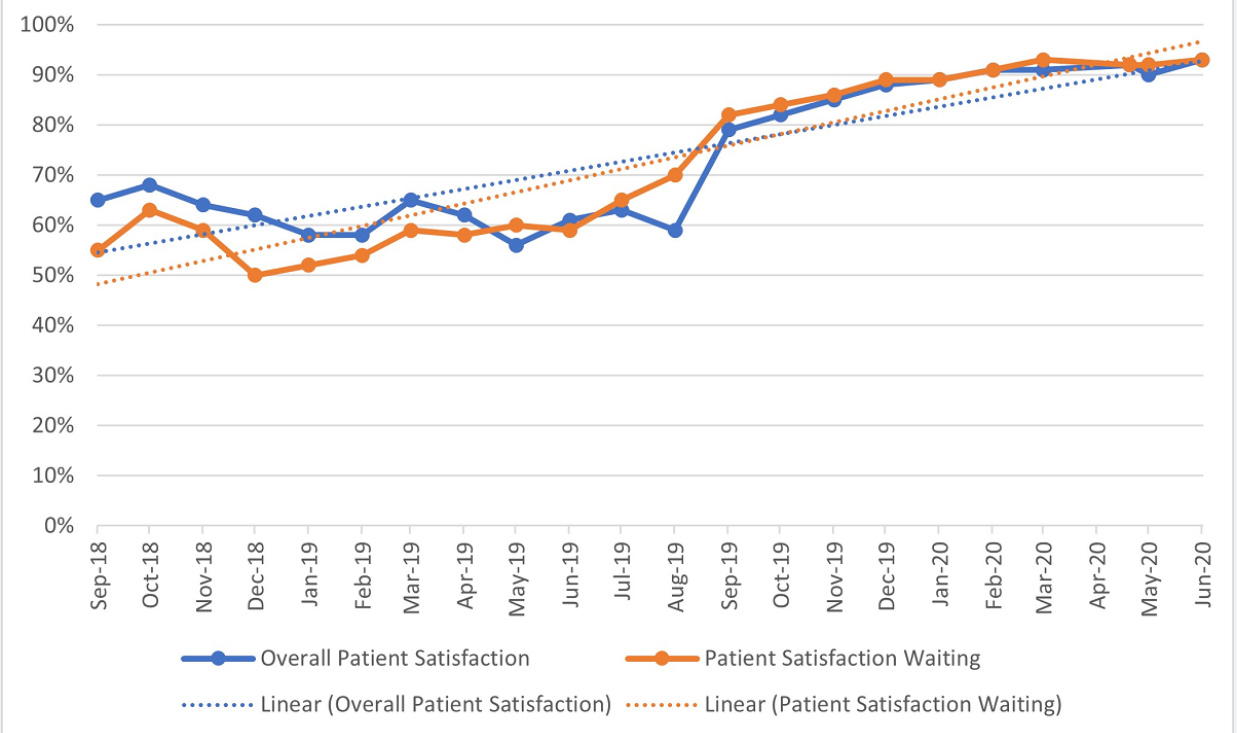
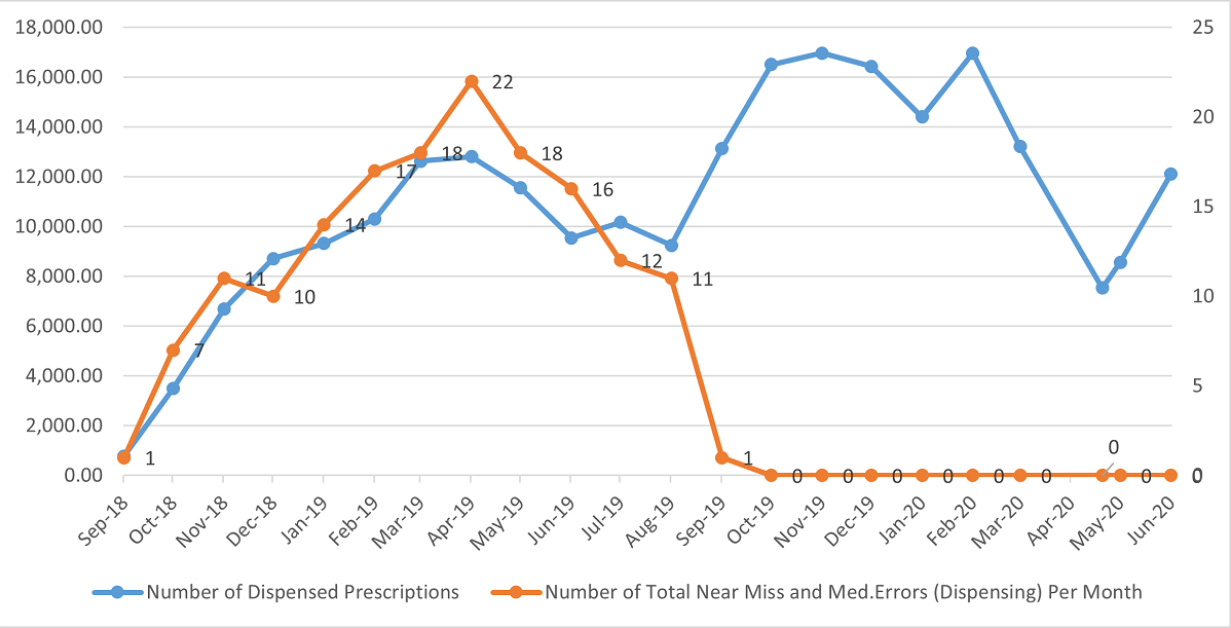
An important priority for patients, particularly outpatients, is the time spent waiting for medications to be dispensed5. The most common method of outpatient dispensing is for original-pack medications to be given to the patient rather than unit-dose or blister-packs. This method has advantages for automation, as it requires less fine manipulation of the dispensed medication and allows for a relatively faster throughput and service to the patient6. A 21-month study was conducted in Saudi Arabia between September 2018 and June 2020 with a go-live for an automated pharmacy system after 11 months. This gave pre- and post-implementation data over an extended period allowing for comparison of equally complex patients with diverse issues of infirmity, age, education, pharmaceutical requirements, and health state.7
Figure 1: Management Processes, Challenges, and Pain Points, in Outpatient Pharmacy Dispensing Mapped alongside Solutions.
This study focused strongly on patient satisfaction using standardized questionnaires in Arabic and English to measure the patients’ experiences which could be completed by patients and carers via tablets and smartphones. There was a substantial difference in patient satisfaction pre- and post-automation, which strongly correlated with waiting time reductions and more ring-fenced time spent with pharmacy professionals. This is in line with a European study that reviewed the factors associated with outpatients’ satisfaction with the services they receive.8
Figure 2: Automation Go-Live in August 2019: Patient Satisfaction with Waiting Time and Overall Patient Satisfaction climbs to over 90%.7
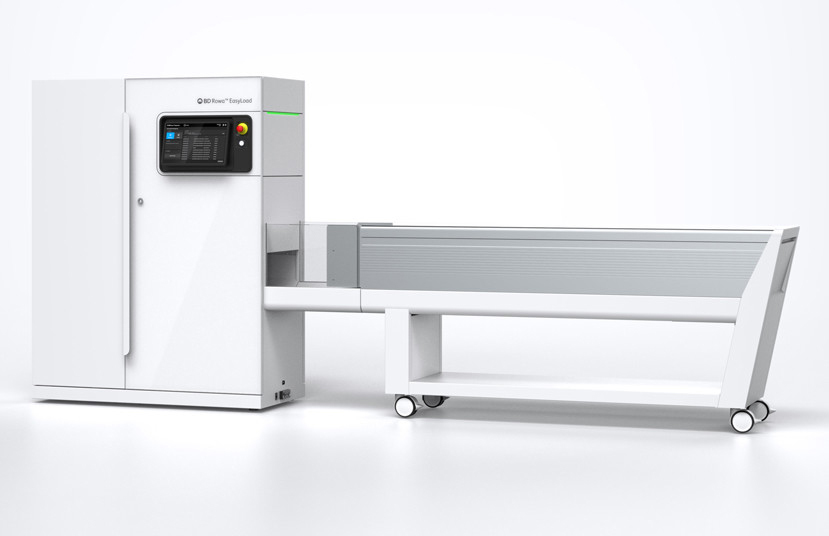
The increase in speed of dispensing by the automated pharmacy leading to these reduced waiting times can be accounted for the nature of ‘picking’ by the pharmacy robot; rapid barcode identification of ordered medications and multi-picking of up to eight medication packages per move makes for a speedy pick up.
Conveyor belts and automated gates leading to spiral chutes can deliver these picked medications directly to patient service points.
The study7 also addressed maintaining medication safety with an increasing outpatient census with growth expected to be 25% per annum and planned for over 5- and 10-year horizons. Against an on-average increasing number of dispensed items, it is notable that the dispensing error rate descended to a near zero rate.
Figure 3: Automation Go-Live August 2019: Medication Error Rate versus dispensed item volume.7
In a study reported in 2022, the Six Sigma method9,10,11 was applied to an outpatient pharmacy automation project in a large facility receiving 500,000 outpatient visits yearly (with an increase of ~15% per year), operating 24 hours a day, and serving metropolitan Riyadh. The project was undertaken to improve patient safety, quality of service, and to reduce costs.12
A key point during the introduction of automation to any human system is to maximize the integration of robotics to the workforce. Mapping processes using the Six Sigma methodology and creating Ishikawa plans before the introduction of automation can be useful methods to improve synchronicity between humans and robotic systems.13 It also helps identify ‘choke-points’ that can be addressed directly by automation, or that require re-engineering of the workflow.
Figure 4: A pre-automation Ishikawa fishbone diagram with input and output deficiencies. 12
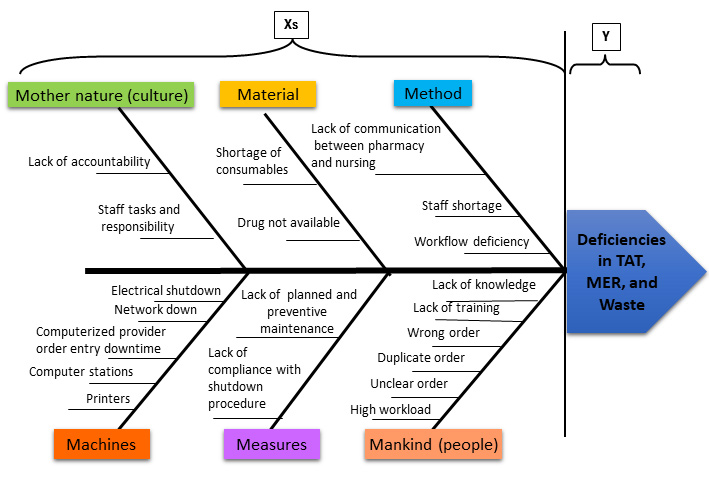
The Six Sigma approach also produces a road map that integrates tracking and monitoring into its process. Tracking of activity in the outpatient department focused on removing non-value-added (NVA) pharmacist tasks and key outcome metrics, including storage, picking and
delivery dispensing rates, patient and prescription load per day, average packs and lines per prescription, and lines held were developed.
The two automated dispensing units were integrated with the hospital’s information technology (HIT) that supports appointments, medication records, and prescriptions.
In this study, post-automation, the total patient time in the department, including the time interacting with the pharmacist for medication education and counseling, dropped from 17.093 to 11.812 digital minutes, with an appreciable increase in patient-pharmacist time. 12
The percentage of incomplete prescriptions dispensed versus orders decreased from 3.0% to 1.83%. The dispensing error rate dropped from 1.00% to 0.24%. During implementation, it was found that NVA tasks that were replaced by automated processes had been responsible for an extensive loss of pharmacist time. The productivity ratio post-automation was 1.26.
When adding stock, pharmacy robots read the expiry dates on drug packages, and thereby reduce waste from out-of-date medications, and can also automatically recognise medications that require refrigeration. Some automated pharmacies have internal refrigerated storage units within them, and their entire stock area is temperature controlled.
Regular inventory is a labor-heavy task in a manual pharmacy. Automated pharmacies have advantages in maintaining a consistent inventory count as each of the actions; direct loading into the robotic-managed storage with barcode reading for medication stock-up and automatic item deduction from stock level upon dispensing is under its control. This means that the inventory balance is a constant and dynamic process. In the 2022 Riyadh facility study12 Medication wastage from expiry was assessed via a ‘basket’ of medications. In this study, wastage cost was reduced by 83.9% post-automation.
From what has been seen in these studies, the time savings achieved, and accuracy of automated dispensing for outpatients are impressive. The studies also indicate that the fuller the integration between systems such as Computerised Practitioner Order Entry, Electronic Medication Administration Record, and the patient’s Electronic Medical Record and automated dispensing systems, the greater are the potential gains for the organisation.
Perhaps what is most important is that our most valuable asset, skilled pharmacists, are freed from non-value-added tasks and can devote their expertise to patient counseling and education. With at home medication error and non-adherence being estimated as being responsible for an estimated 14.7% of emergency room admissions in Saudi Arabia per year,14 it is clear that the patient, and their medication education needs must be at the centre of any outpatient automation strategy.

References:
1. Hynniman C, Lamy P. Outpatient pharmacy automation. American Journal of Hospital Pharmacy 1967; 24. 18-21.
2. Oñatibia-Astibia A, Malet-Larrea A, Larrañaga B, Gastelurrutia, Calvo B, Ramírez D, Garay, et al. Tailored interventions by community pharmacists and general practitioners improve adherence to statins in a Spanish randomized controlled trial. Health Serv Res 2019 Jun 07;54(3):658-668.
3. Ahtiainen H, Kallio M, Airaksinen M, Holmström A. Safety, time and cost evaluation of automated and semi-automated drug distribution systems in hospitals: a systematic review. Eur J Hosp Pharm 2019 Mar 19;27(5):253-262.
4. National Pharmacy Association. NPA medication safety update (MSO report). NPA medication safety update (MSO report) Quarter 4 2019 (England). 2019. URL: https://www.npa.co.uk/news-and-events/news-item/npa-medication-safety-update-mso-report-quarter-4-2019-england/ [accessed 2022-10-19]
5. Tam V, Lim M. Patients’ Perceptions and Expectations of Outpatient Pharmacy Services in a Teaching Hospital. Int J Pharm Prac 1997;5:128-132.
6. Tan W, Chua S, Yong K, Wu T. Impact of pharmacy automation on patient waiting time: an application of computer simulation. Ann Acad Med Singap 2009 Jun;38(6):501-507.
7. Momattin H, Arafa S, Momattin S, Rahal R, Waterson J. Robotic pharmacy implementation and outcomes in Saudi Arabia. A twenty-one month review. JMIR Hum Factors. 2021 Jul 23.
8. Martínez-López-de-Castro N, Álvarez-Payero M, Martín-Vila A, Samartín-Ucha M, Iglesias-Neiro P, Gayoso-Rey M, et al. Factors associated with patient satisfaction in an outpatient hospital pharmacy. Eur J Hosp Pharm 2018 Jul 16;25(4):183-188.
9. Niñerola A, Sánchez-Rebull MV, Hernández-Lara AB. Quality improvement in healthcare: Six Sigma systematic review. Health Policy 2020 Apr;124(4):438-445.
10. De Koning H, Verver J, van den Heuvel J, Bisgaard S, Does R. Lean Six Sigma in healthcare. J Healthc Qual. 2006;28(2):4-11.
11. DelliFraine J, Wang Z, McCaughey D, Langabeer J, Erwin C. The use of Six Sigma in health care management: are we using it to its full potential? Qual Manag Health Care 2014;23(4):240-253.
12. Al Nemari M, Waterson J. The Introduction of Robotics to an Outpatient Dispensing and Medication Management Process in Saudi Arabia: Retrospective Review of a Pharmacy-led Multidisciplinary Six Sigma Performance Improvement Project. JMIR Hum Factors. 2022 Oct 11;9(4):e37905.
13. Van den Heuvel J, Does R. Dutch hospital implements Six Sigma. Six Sigma Forum Magazine 2004;4(2):11-14.
14. Al-Olah Y, Al Thiab K. Admissions through the emergency department due to drug-related problems. Ann Saudi Med 2008;28(6):426-429.














