Pandemic Response: Maintaining Effective and Safe IV Infusion Therapy for Critically Ill and Isolated Patients

Lisa Gangol. RN, BSN. Beckton Dickinson. Senior Clinical Resource Consultant. Medication Management Solutions. Eastern Europe, Middle East & Africa.
Natalie Samuda. RM, BSc. Becton Dickinson. Senior Clinical Resource Consultant. Medication Management Solutions. Eastern Europe, Middle East & Africa.
James Waterson. RN, M.Med.Ed. Becton Dickinson. Medication Safety Manager, Eastern Europe, Middle East & Africa. James.Waterson@bd.com
The magnitude of IV medication error even under ‘normal’ conditions is large (*). Smart Pumps with Dose Error Reduction Systems (DERS) reduce this risk with the application of hard limits for dose/rate, concentration, and duration of continuous and intermittent medications (#). The Covid-disease pandemic’s requirement for strict isolation of large numbers of patients has made maintaining the Rights of IV medication administration: patient, medication, dose, route, timing, and documentation, increasingly difficult.

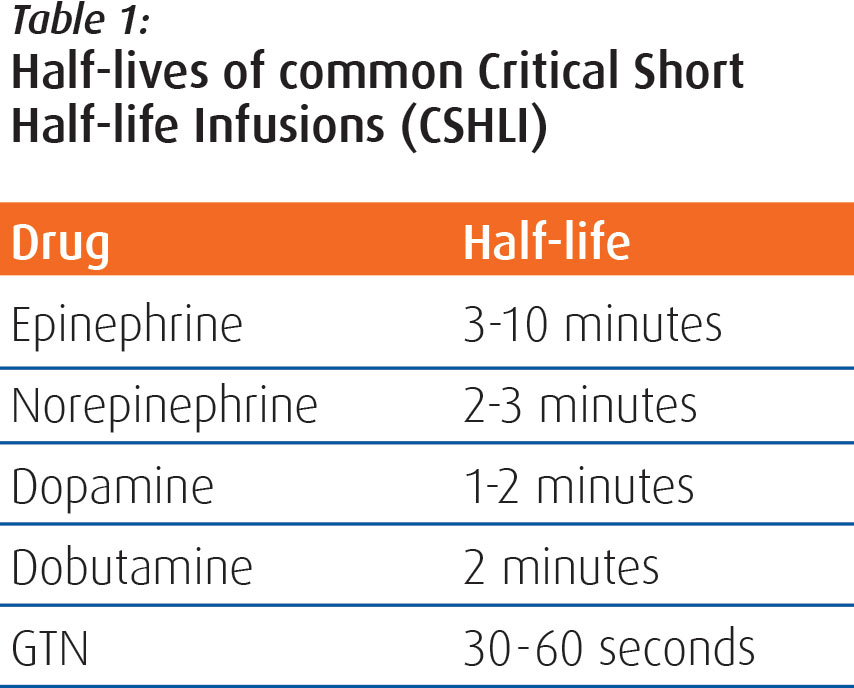
There is also the Right Maintenance of continuous critical short half-life infusions (CSHLI) such as noradrenaline or glyceryl trinitrate. Of course, with critically ill Covid-disease patients in the ICU any prolonged interruption of CSHLI infusion delivery could be fatal. Monitoring of these infusions is vital for isolated ICU patients, as nursing staff must respond promptly to any infusion alarm, and certainly within the plasma half-life of these medications if serious cardiovascular events are to be avoided. Some typical half-lives of CSHLI are given in Table 1.
A three-year retrospective study in The University Hospital of Antwerp, Belgium identified that centralised monitoring of isolated neonates in an NICU with 60 single-rooms reduced nurse reaction times to CSHLI alarms by 31% and reduced the total number of alarms that nurses are exposed to by 56.25%. (**) We therefore recommend central monitoring of all infusions delivered to isolated patients. This has an extension beyond the pandemic to immunocompromised critical patients who require protective isolation. The use of wireless pumps in single rooms that can transmit their infusion data and any alarms to a centrally based monitor is extremely valuable in this respect.
To reduce nursing time for IV bag changes and intermittent IV medication administration spent inside rooms of SARS-CoV-2 virus infected patients some facilities have adopted the use of long extension lines that allow the patient’s pumps to remain outside of the isolation room. This practice does have some issues that must be considered to maintain safety, infusion continuity and accuracy. This includes considerations on how to run the IV line to the patient. Running the IV line under the door and across the room’s floor, and taping and padding it to prevent tripping or dislodgment, is not ideal but does provide protection of the line and a visual warning of its presence. (##) However, the technique may cause issues of pressure gradient changes affecting occlusion alarms, accumulation of air in the line due to the low level of the line in relation to the pump and the patient, and of rate accuracy. This is related to a question of physics. In nonideal fluid dynamics the Hagen-Poiseuille law gives the pressure of an incompressible fluid flowing through a long cylindrical pipe or tube of constant cross section. The law states that the steady-flow velocity (Q) of a fluid through a narrow tube (such as an IV set or a catheter) will vary in relation to the pressure drop (Δp), to the radius (R) of the tube, to the length (L) of the tube, and to the viscosity (μ) of the fluid in the line. In standard fluid-kinetics notation this is expressed as:
Q =π∆Pr4 / (8µL)
Where:
- Q is the volumetric flow rate.
- Δp is the pressure difference between the two ends of the infusion line.
- L is the length of pipe or tube.
- μ is the fluid dynamic viscosity.
- r is the line or catheter radius.

Smart pumps are accurate, but long lines can then, in theory, increase siphonage in the case of large bore lines and increase downstream pressure when microbore lines are used. It is important to maintain the recommended height of the infusion bag above a large volume pump (this is usually 50 centimetres) and any unnecessary resistance in the downstream line should be reduced by keeping the extension set additions as limited as possible to achieve a safe working distance, and infusing through as large an IV catheter as possible. Priming of long extension lines can be undertaken by gravity, but it is often easier to control the prime by using the pump.

Another consideration with long lines is that downstream occlusion pressure limits may need to be increased to avoid nuisance alarms, particularly at higher rates, due to higher volumes being forced through long narrow tubing. This can be done by the user at the bedside, but when we have wireless-connected smart pumps in a facility changes to default pressure alarms configurations can be made centrally and distributed rapidly via the network to all pumps. Smart pumps should also have an option of occlusion pressure limits that are dynamic, meaning that the flow rate automatically determines and alters the downstream occlusion pressure alarm. In this case, with long extension lines, this mode can be considered at rates above 30 ml/hr. Of course, critically ill Covid-disease patients are likely to be receiving multiple infusions through one IV access line, and if the disease causes Systemic Inflammatory Response Syndrome or there is a secondary systemic sepsis, there may be an emergent need for rapid delivery of IV fluids. In this situation a dynamic occlusion alarm is of real value, as it will reduce the number of nuisance occlusion alarms and assist with infusion continuity. Pumps with auto-pressure features which, on activation, set a margin of 30 mmHg above the patient-line pressure also allow for a rapid user response to occlusions alarms.
Independent studies on the cleaning of long-lines and their materials suggest that wiping a PVC extension set 2-3 times daily with 70% isopropyl alcohol solution has minimal impact on the line’s function and performance (i.e. there will be no weakening leading to excess kinking or excessive compliance on the line). The risk of isopropyl alcohol entering the fluid pathway is negligible. It is therefore expected that the PVC IV extension sets would still deliver their critical function with minimal risk to clinician or patient. With repeated disinfection of PVC extension sets clinicians may note visual defects on the line’s surface and that it feels ‘tacky’. This has no impact on the line’s performance and is limited to the exterior of the line. (^)
Administration of intermittent infusions with long lines requires that we know the priming volume for the entire length of the tubing when programming infusion rates and flush volumes. Nurses should consider priming the set with the medication rather than with normal saline or dextrose, to facilitate prompt delivery. Post-medication flushes should be given at the same rate as the medication. This is best achieved with well-constructed DERS libraries with pre-set durations of delivery for each medication and smart pumps with a ‘restore’ function for ensuring accurate rate/volume delivery of the flush.
A large capacity DERS library with multiple profiles can allow for a specific library for critically ill Covid-disease patients, giving rapid and easy access to specific medications used to care for these patients along with specialist concentrations and higher dilution medications to be used with long-lines. The Covid-disease pandemic has also caused supply shortages in key medications, such as Fentanyl, the ability to rapidly update alternate medications in the DERS library, such as substituting Propofol 2% for 1%, and to deploy the new library remotely via wireless allows facilities to respond and adjust rapidly to supply challenges, and to emergent changes in treatment protocols such as the new protocol for Dexamethasone use in Covid-disease.

IV medication administration commonly requires a two-nurse check. With highly infectious isolation patients this can potentially expose two nurses to the risk of infection during patient identification. In highly developed IV infusion medication safety systems the second nurse can be replaced by barcode medication administration (BCMA) during which the smart pump, via a bidirectional wireless communication with the patient’s electronic mediation administration record (EMAR), undertakes the bedside checks of right patient, right medication, and right timing, and automatically documents administration in the patient’s EMAR.
Appropriate cleaning and decontamination of pumps between patients, and on a regular basis, is a both vital component of pandemic planning, as well as being central to any ‘standard’ infection control plan. Selection of infusion pumps is a factor here. There should be no difficult to access areas that can harbour contaminant and that cannot be exposed to disinfectant material. This includes plunger grips on syringe pumps and line or cartridge loading spaces on large volume pumps. Furthermore, the pump’s body must be not be degraded by cleaning products that can fight the SARS-CoV-2 virus.
New polymers released in the last few years for pump manufacture have considerably broadened the cleaning products that can be used without fear of damage to the device. If there is any doubt over the use of a cleaning product, the manufacturer’s local agent should be contacted. We have found that a review of the Material Safety Data Sheet of combination cleaning products has allowed us to reassure customers over the continued use of their chosen cleaning product.
The care of patients in isolation stretches a facility’s physical resources but demands on resources do not stop at devices and equipment, there is also a high demand for Critical Care clinicians as ‘pop-up’ pandemic critical units are opened. Facilities have had to quickly cross-train existing staff and recruit new staff to ease the burden. Clinical facilitators are tasked with upskilling nurses who usually work non-critical care areas to care for critically ill patients. The training and education of staff is essential to maintaining patient safety. Facilities benefit from partnerships with device vendors, providing educational resources and clinical trainings to ensure best practices. Infusion therapy during a pandemic is multi-faceted and challenging, but patient safety does not have to be compromised even under the strictest of isolation procedures. Engaging with your infusion device vendor to seek expert advice, the application of technology, and creative strategies that build on, or adapt, existing safeguarding processes and strategies are the keys to keeping both critically ill patients, and the staff caring for them, safe.
References.
*Lahue et Al. National Burden Of Preventable Adverse Drug Events Associated with Inpatient Injectable Medications Healthcare and Medical Professional Liability Costs. American Health Drug Benefits 2012: (5)7. 1-10.



















